Diseases have been a part of humankind for many years. Our forefathers were victims of major disease outbreaks
of smallpox, bubonic plague, and influenza. Now, we are a part of a historical disease outbreak on the planet, the COVID-19 pandemic. The biological organisms that proved themselves capable of bringing humans down to their feet are microorganisms.
The microbial world comprises some organisms that are beneficial for us, and some that are harmful. They are called pathogens, including bacteria, viruses, fungi, and parasites. Pathogens disrupt the normal functioning of
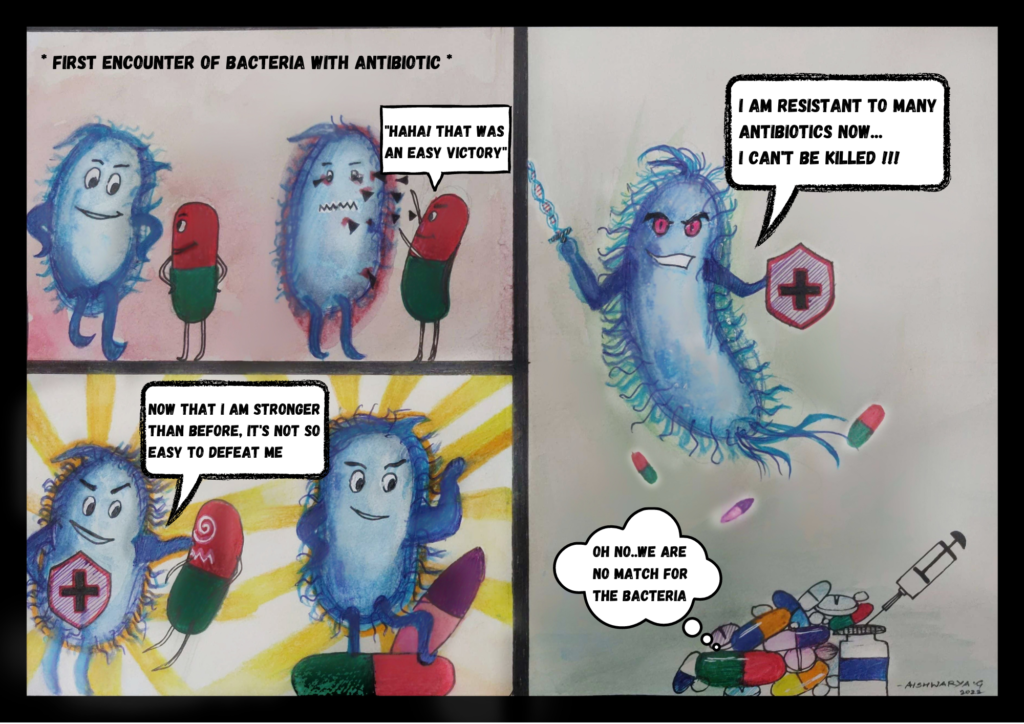
the body, leading to the development of diseases. Humans become victims of new pathogens and diseases every day. Research focuses on producing medicine or drugs to treat them. Antimicrobials are drugs that focus on inhibiting growth or killing the pathogens affecting the body. Every new creation has its pros and cons. The drugs made to treat life-threatening diseases are now proving ineffective because of antimicrobial drug resistance, an
evolutionary process leading to modification in the characteristics of the pathogens with time. This evolution is
favorable to pathogens, but not to us.
Let’s understand microbial drug resistance through a simple example. Moving to a hostel seems awful for all of
us, and what makes it even more dreadful is the food. It gets a lot of time to get acquainted with the menu and the taste. Most of us don’t like it at first and also might end up falling sick. Eventually, we all get used to that food, and we don’t end up falling sick frequently. When we consume a dish entirely different from our usual palate, for instance, when visiting a country with entirely different cuisine, our gut might get upset at first, but slowly adapt itself to the new food items consumed by us. With time, our gut becomes “resistant” to falling sick from that food.
Similarly, microbes exposed to antimicrobial agents evolve so that they become resistant to the drugs’ mechanism
of action. Some of these mechanisms include inhibition of the bacterial cell wall synthesis, inhibiting the activity of any important enzyme or protein, or disturbing any metabolic pathway. One of the most common diseases, tuberculosis, has gradually achieved antimicrobial resistance with the origin pf Multiple Drug Resistance (MDR)
Tuberculosis. The evolution of the MDR strain of TB has led to an increase in deaths because of this disease, especially in developing nations. According to the WHO, Antimicrobial resistance is one of the top 10 global public health threats.
Let’s dive into other aspects of this phenomenon: what triggers pathogens to evolve themselves to be resistant? Is there any solution for the same?
The earth is continuously changing since its inception, and so are its residents. Microbes have inhabited this planet for billions of years. They have less genetic material as compared to human beings, and they procreate within a small amount of time. The E.coli bacteria have about 4000 genes, which are DNA sequences coding for proteins and other biological products, whereas humans have approximately 25,000 genes. E.coli can duplicate itself in 20 minutes while humans take up to 9 months to produce a newborn. These features help microbes change themselves and adapt quickly to environmental changes compared to complex organisms like humans.
With antimicrobials and their easy access, people now rely on them for even the mildest of symptoms.
Indiscriminate use of antibiotics for daily ailments without prescription is a problem. Everyone wants a quick fix to discomfort and diseases. This makes people self-medicate. If one medicine doesn’t work, they jump on to the next. General practitioners prescribe multiple drugs to patients reporting symptoms such as cold, fever, cough, headache, etc. without conducting proper diagnostic tests. Antimicrobials are now considered a first-line treatment for any infection. People buying medicines without a prescription is not uncommon these days. This adds fuel to the fire of antimicrobial resistance.
We see several commercials for antiseptics and disinfectants claiming to provide 99.9% protection against germs. Such advertisements endorse complete hygiene in our surroundings as if sweeping away all microbes from the earth is possible and is the only acceptable way of survival. The microbial world eventually gets exposed to selection pressure, wherein certain environmental factors affect the ability of the organisms to survive by bringing about changes in their genetic makeup. The continuous exposure to their enemies, the antimicrobial drugs leads to them developing resistance to the effects of these drugs. Indiscriminate use of such drugs exposes the
microbial world to a course of evolution to develop resistance against the same. Hygiene is extremely important, especially when preparing food items or when using washrooms, but disinfecting every surface we touch all the time makes our immune system more and more vulnerable to infectious diseases. Disinfectants contribute to the selection of resistant strains of bacteria, resulting in their rise.
To prevent antimicrobial resistance, we can work upon certain habits that we have developed over the years contributing to drug-resistant pathogens. Our constant urge to self-medicate and ‘immunize’ ourselves as quickly as possible is best avoided. Healthcare professionals, pharmaceutical companies, hospitals, and other stakeholders can focus on making people aware of the magnitude of the danger of antimicrobial resistance. Minimizing the usage of drugs is the most crucial way to mitigate the development of drug resistance. Drugs need to be taken after a proper diagnostic test, in the exact prescribed dosage and complete time period, for them to be effective without consequences. Whenever consuming antimicrobial drugs, it is crucial to follow the specifications prescribed by the doctor.
Rome wasn’t built in a day. Changing habits of people over the usage of antimicrobial drugs won’t change in a matter of weeks or months or a few years. Combating antimicrobial resistance will require consistent efforts by the public and stakeholders over a long period. Equal participation of all of us will help prevent antimicrobial resistance occurring in present-day pathogens and novel ones occurring tens of thousands of years from now.
Sources:
1. Antimicrobial resistance. (2021, November 17). WHO. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
2. Michael, C. A., Dominey-Howes, D., & Labbate, M. (2014). The Antimicrobial Resistance
Crisis: Causes, Consequences, and Management. Frontiers in Public Health, 2.
https://doi.org/10.3389/fpubh.2014.00145
3. 1997: E. coli Genome Sequenced. (n.d.). Genome.Gov. https://www.genome.gov/25520386/online-education-kit-1997-e-coli-genome-sequenced#:%7E:text=to%20prevent%20infection.-,The%20E.,and%20contains%20approximately%204%2C000%20genes.
4. NHGRI. (2019, March 13). Human Genome Project FAQ. Genome.Gov. https://www.genome.gov/human-genomeproject/CompletionFAQ#:%7E:text=The%20human%20genome%20contains%20approximately,the%20instructions%20for%20making%20proteins.
. . .
Writer
Sreelakshmi S Kumar
Editor
Namrata Pandit