COVID-19 is one of the biggest global health crises of the 21st century. This pandemic has had severe and far-reaching impacts on the health system, economies, and societies. Countless people have died. They lost their livelihood. Families have been strained. The majority of the population is thrown below the poverty line. The young population have missed out on learning and socializing. But little has been said about the impact of the pandemic on mental health.
The Mumbai Municipal Corporation’s mental health helpline received a massive 45 thousand calls during the first two months of the pandemic. Out of the 45 thousand calls, 82% were citizen complaints about anxiety, loneliness, restlessness, and depression, with the remainder complaining about irregular sleep and exacerbation of pre-existing psychological problems.
Lockdown is the world’s biggest psychological experiment, and we will pay its price.
The first line you will encounter in the guidelines given by the government of India for treatment protocol during the COVID-19 pandemic.
But one thing that this pandemic has underscored is mental health. If you ever tell your parents, I want to visit a psychiatrist. Their answer will be to wake up early and use your mobile less. Period. No need for a psychiatrist. The bitter truth of our society is that people avoid going to counselling and therapy due to the stigma attached to them.
After the COVID-19 outbreak, scientists, doctors, governments, and everyone around the world was baffled. What to do? How to stop the spread of this virus? How to treat the infected ones? Governments all over the world chose a zero contract policy, also known as lockdown. Fancy word quarantine. It slowed down the spread of the virus and bought us more time to gather data, study, and find a cure. Today we are getting back on track with the profound vaccine. Thanks to the tireless efforts by everyone involved in this quest for a cure. Are we really back on track? Physically we might be, but mentally?
Sometimes all you need is a warm hug from your loved one. Touch is magic. It’s the sweetest and warmest medicine you could ever ask for. But this lockdown cut off the human touch totally. Studies have shown declining cognitive function with reduced human contact.
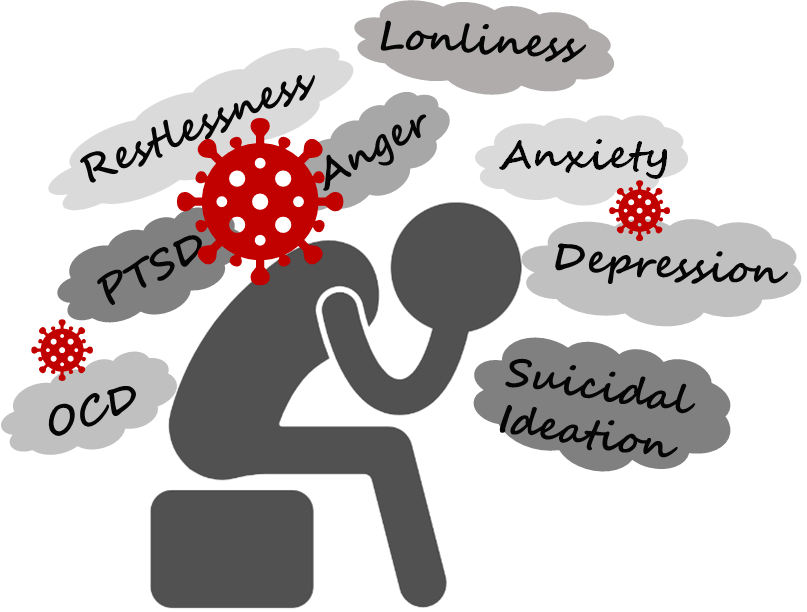
Front-line health workers and law and order personnel who are exposed to trauma, grief, and distress for a long period of time develop issues like post-traumatic stress disorder (PTSD), loneliness, obsessive-compulsive disorder (OCD), anger, and suicidal ideation.
A person suffering from depression feels a constant low mood. People lose interest in their daily working routine. Excessive sleeping or no sleep at all is observed in people suffering from depression. Change in appetite has been linked to weight loss and excessive weight gain.
People suffer from post-traumatic disorder, most commonly known as PTSD, when they experience a traumatic event in their life. They isolate themselves from the external triggers that can remind them of that event. Nightmares, intrusive images, and flashes of the event are perceived by people. They re-experience the trauma by getting vivid flashbacks.
The adolescent age group is the most vulnerable age group of all. Exposure to high-stress situations causes long-term adverse effects on their mental and physical health. Lack of emotional processing, suicidal behavior, substance abuse, altered eating habits, and obesity are observed. With underdeveloped brain circuitry, leading to reduced concentration levels.
In the second wave of the COVID-19 pandemic, the health system in India was literally brought to its knees. In the month of April of the current year, there was a state of fear, panic, and extreme stress. Because there was a sudden spike in deaths from the pandemic and a record rise in new cases. But this is not just a picture of one month. The past years have seen a rise in nervous disorders and mental disorders worldwide.
The rule of halves can be used to understand the grave nature of mental health diseases. According to Rule 1, half of the people with disease are not known. Half of those who are known are not treated is the second rule. And the third rule is that half of those who are treated are not controlled. If we sum up, the total percentage of people actually getting treated and recovering is far less than the actual number.
Over the years, India has become one of the most depressed countries in the world. Citizens who do not get enough help or need help, turn to alcohol or drugs, become addicted and turn to violence. The continued neglect of mental health has led to a stigmatization of mental illness and a lack of information about it.
Such an effect was prominent during all the pandemics in history. In the 2003 SARS outbreak or in the 2013 Ebola outbreak. More than 50 percent developed depression who recovered from the infection. The new digital age has added to mental stress. The capacity of the resources is stretched and all the related mechanisms are exhausted. The past year has starkly demonstrated the importance of access to overall mental health care. A striking 9 crore of the country’s population is facing mental illness.
Treating mental illness is not a cakewalk. It’s a team effort involving the patient, doctor, and patient’s relatives. A wide range of drugs are available, from sedatives to selective serotonin and norepinephrine reuptake inhibitors (SNRI). They act at the synapses of neurons, where these feel-good hormones are secreted. They prevent their metabolism and keep their levels high, elevating a person’s mood. Sedatives and hypnotics like diazepam, alprazolam, and amitriptyline help to calm the mood of a person. Alongside drugs, behavioral therapy, yoga, and meditation are popularly used to treat mental health conditions.
The world does not have the necessary resources to handle a pandemic of such magnitude. But when it comes to mental health complications, the situation looks much worse. This pandemic was also significant in terms of creating awareness and information about mental health. Those who needed self-help and help managing their own emotions, faced a state of extreme confusion. Fighting this long-standing issue requires targeted, cross-cutting efforts and all-out investment from all stakeholders globally as the availability of funds is less likely. Industrialists, philanthropists, and above all, governments should come together to overcome the problems created by the pandemic and secure the future of humanity.
Reference:
1. https://www.who.int/teams/mental-health-and-substance-use/mental-health-and-covid-19
2. https://www.orfonline.org/marathi/mental-health-in-times-of-covid-lessons-we-refuse-to-learn-86977/
3. https://www.the-scientist.com/news-opinion/covid-19-linked-to-neural-changes-69779
4. https://www.the-scientist.com/features/how-social-isolation-affects-the-brain-67701
5. https://www.who.int/news-room/feature-stories/detail/the-impact-of-covid-19-on-mental-health-cannot-be-made-light-of
6. https://www.the-scientist.com/editorial/our-aching-brains-69233
. . .
Writer
Apoorva Koli
Illustrator
Deeksha Waghela
Editor
Gauri Panzade

