The human body is a fascinating work of biology, full of cells and organ systems. Despite their complexity, our bodies are fragile and can be damaged by different accidents, infections, diseases, and syndromes. Some of them can be cured or managed thanks to science and technology, but sometimes the damage is so severe that the part or organs can no longer function, and the only choice is to have them replaced. Such a replacement or transfer of cells, tissues, or organs from one site or person to another is called transplantation. Many disorders, including leukaemia, non-lymphoma, Hodgkin’s sickle cell disease, and cancer, can be cured through transplantation. All of us are similar and share 99.9% (yes, 99.9%) of our genes, and yet we can’t just give parts of our bodies even if we wanted to. Why is there an organ shortage? What makes transplants so tricky? The answer? It’s our immune system.
Yes, you read that right. Our immune system, the pillar of the body’s defence, is what hinders the process. So many things in nature have the ability to harm us. Because of this, our immune system has evolved to be the epitome of paranoia. It recognizes transplanted cells as foreign entities and, like experienced assassins, strives to remove them as quickly as possible, rendering the transplant ineffective. If all human cells are similar, why does the immune system recognise transplanted ones as foreign? This is because transplanted cells and organs have something called antigens. Antigens are foreign entities that are recognised by our immune cells. While a transplant may have many antigens on its surface, there are two antigens that our immune cells attack the most. These are the self-blood group antigens and the MHC antigens.
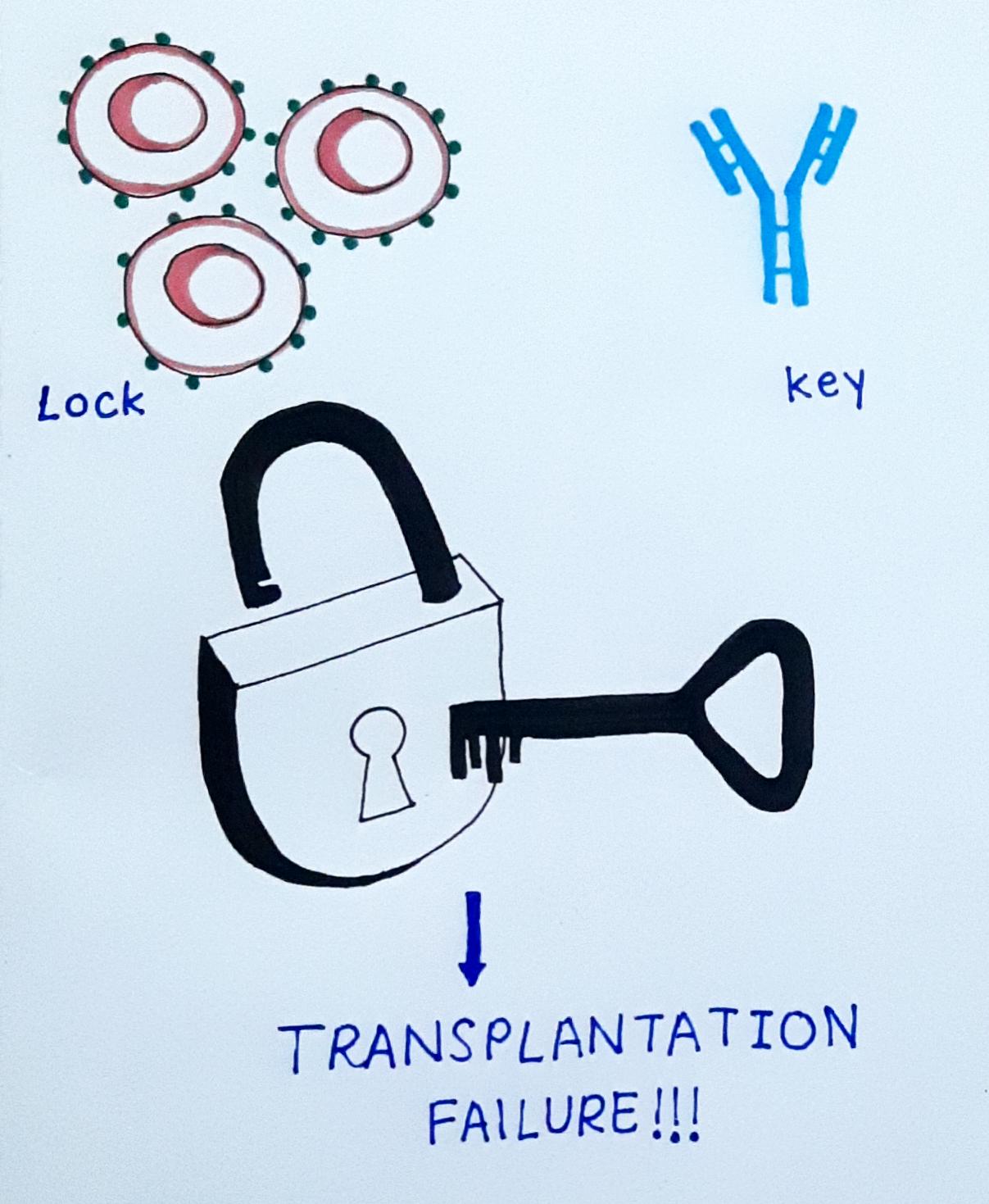
Did you know that the A, B, AB, and O blood groups are based on the self-antigens present on RBCs? Don’t worry, your body won’t attack its own cells. An A blood type person has A antigens on their RBCs and some body cells but no anti-A antibodies in their blood. Antibodies bind to antigens and help immune cells recognize and kill them quickly. Think of antigens and antibodies as locks and keys, respectively. If our (key) antibody binds to the (lock) antigen, it releases a cascade of reactions, leading to the destruction of the transplant. When an A blood group antigen recipient receives a transplant from a B blood group antigen donor, the recipient’s antibodies bind to the donor cells, causing the transplant to be rejected quickly. This is why matching of blood groups is essential.
The second antigen, MHC, stands for Major Histocompatibility Complex. The MHC is a tiny protein found on the surface of all cells in an individual’s body. Each MHC is synthesized with the help of several genes, each of which exists in many forms. Different forms of the same gene are called alleles. Consider the MHC genes to be boxes, and their many forms to be coloured balls. Each box (gene) needs to have a certain ball (an allele). Now think of the many permutations and combinations possible! mind-numbing, isn’t it? A person could have a red-coloured ball in box 1, whereas another could have a blue ball in box 1. It’s amazing that only 0.1% can account for so many differences between us. In order for a transplantation to occur between two people, the maximum number of balls in all the boxes should match between them. Such a matching of alleles is called tissue typing. If a greater number of alleles don’t match, there is a greater chance for the transplant to be recognised as foreign.
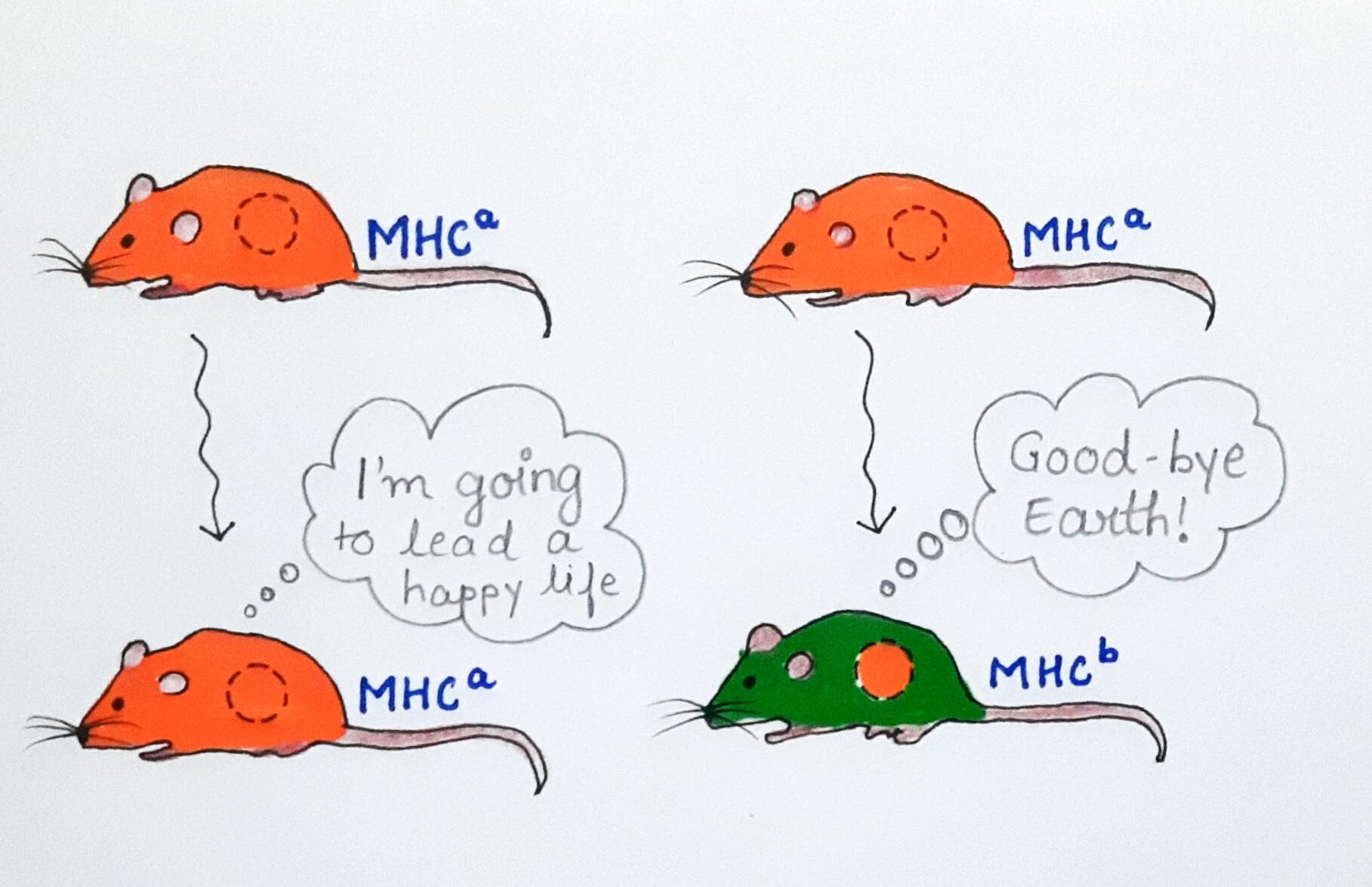
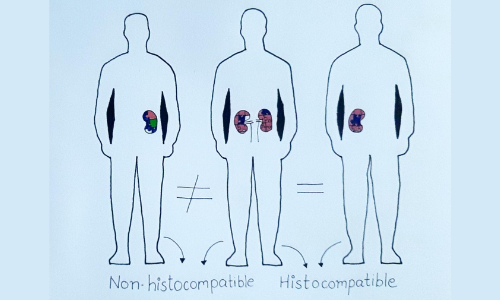
This is why family members are the first choice as donors, since we are all related genetically. We inherit one set of genes from each parent, and thus, our parents will definitely match half of the alleles in our body and can be potential donors. If you’re a twin, you’re in luck! There is an extremely small possibility that transplants will be rejected because of your genetic similarities. Transplants between individuals are effective if the majority of their antigens match, and such transplants are referred to as histocompatible transplants. Histo-incompatible transplants are those that have large antigen differences and have a low success rate. The success of a transplant also depends on the organ being transplanted. Some parts of our body, like the cornea of our eye, can’t be accessed by the immune system. Since they are located in a confined area of the body where our immune cells cannot reach, they have a higher success rate than other body parts in terms of transplantation.

Despite its challenges, transplants have altered the way medicine is practiced and helped to prolong the lives of many people. With the use of immunosuppressive medicines, we have successfully transplanted cells and organs with partial matches. Chemicals such as prednisone, dexamethasone, cyclosporin, don’t let our immune system work properly. It primarily targets T cells, which are the main antagonists to transplants, allowing transplanted cells to live longer. However, these medications have a lot of adverse effects and can’t be given to patients for long periods of time, which leads to the transplant being rejected over time. With the immune system weakened, the body is vulnerable to other threats like infections. The drugs also affect the cell cycle, thus leaving the patient at a risk for cancer as well. In spite of successful transplants, over time the body will eventually reject the part, and will need a new transplant. This is what causes the organ shortage we see in today’s day and age.
Science has always been a sign of hope for humans, and is no different in this case. New approaches are being investigated, such as using xenotransplants (pig’s heart) and creating organs with stem cells, to prevent the human body from rejecting the transplant while simultaneously reducing our need for immunosuppressant medicines. Despite the numerous threats, humanity has the will to fight, and with the help of technology, we will overcome the transplantation dilemma, saving many lives.
REFERENCES:
Owen, J. A., Punt, J., Stranford, S. A., Jones, P. P., & Kuby, J. (2013). Kuby immunology (7th ed.). New York: W.H. Freeman.
. . .
Writer
Jwalanthi Sundaram
Editor
Gauri Panzade
Illustrator
Shruti Morjaria