This is about a disorder which is quite prevalent among women of reproductive age. Mostly people possess limited information about the same, consequently giving birth to all sorts of stigma and myths surrounding the condition. Yes, I am talking about PCOS, an acronym for Polycystic Ovarian Syndrome. It is a condition which involves hormonal imbalances in the woman’s body, accompanied by numerous fluid filled sacs, or cysts appearing in the ovaries.
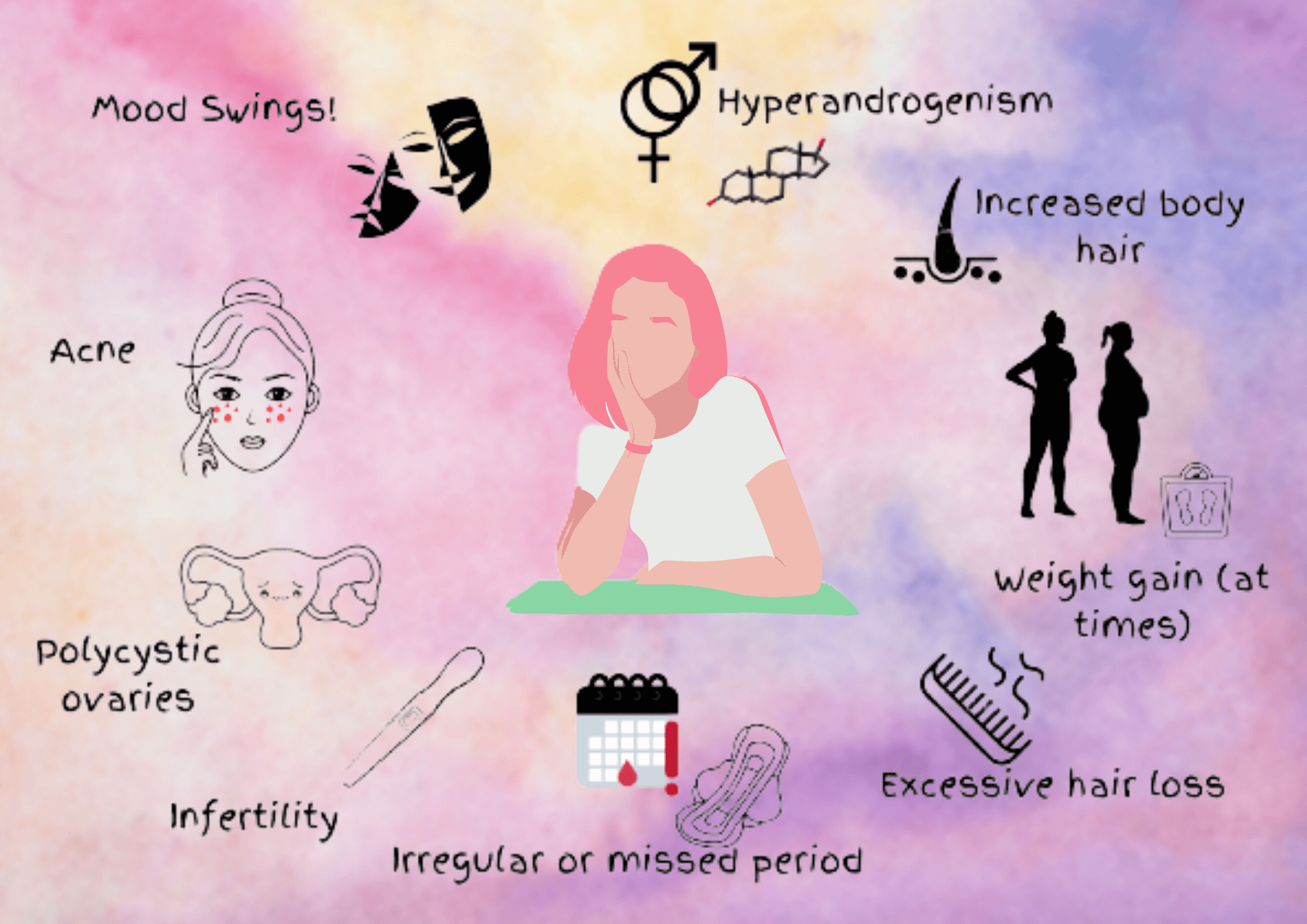
PCOS involves higher level of androgens or male sex hormones in the body, irregular menstruation, and polycystic ovaries. Eventually, the person may start suffering from irregular periods, hirsutism (excessive hair growth on face, chest, back, etc.), obesity, thinning of hair and hair loss, acne, dark patches on skin, etc. One important thing to be considered is that the severity of these symptoms tends to vary between individuals. According to the 2003 Rotterdam consensus criteria, 2 out of the 3 following symptoms need to be present to diagnose PCOS:
- Irregular menstruation
- Hyperandrogenism
- Polycystic Ovaries
Other diagnostic criteria are also considered for this condition. These multiple criteria have undoubtedly limited the accuracy estimation PCOS prevalence among the population. Existing also say that many women remain undiagnosed and so the actual prevalence maybe higher than what is seen lately. Therefore, proper estimation calls for a proper diagnostic criterion.
If the symptoms aren’t controlled or treated properly, it may lead to complications like diabetes, cardiovascular diseases, difficulty in conceiving, increase in cholesterol and triglyceride levels, sleep apnea, depression, and sometimes endometrial cancer. It should be noted that these complications do not always develop since they also vary from person to person.
There is skepticism regarding the factors that cause PCOS. There are certain factors which contribute to its genesis which includes genetics and excess levels of insulin that can subsequently lead to excess androgen. If there is a family history of developing PCOS, the successive generations may be vulnerable to the same. Also, studies suggest there isn’t one but several genes whose cumulative effects determine different levels of symptoms and complications in different women. Of course, the influence of genetics works along with the environmental factors and lifestyle.
One of the hormones predominantly associated with this condition is insulin. This protein, made of 51 amino acid residues, is secreted by the beta pancreatic cells. Now most of us know its particular function, which is none other than reducing blood glucose levels. This is regulated in coordination with glucagon, which is another hormone by pancreas and insulin’s antagonist. Well, the role of the hormone doesn’t end here. Insulin promotes formation of glycogen in the liver which is the storage form of glucose and fat synthesis from glucose in the adipose tissue in the form of triglycerides, which refers to body fat. It also inhibits the breakdown of triglycerides and proteins in the body, reduces glycogen breakdown, enhances amino acid uptake, et cetera, et cetera! Okay, my point here is that insulin does much more than just reducing amount of glucose in our body. Therefore when insulin resistance is present in a woman with PCOS, it can manifest in different ways.
Insulin resistance occurs when the body cells aren’t sensitive to normal insulin levels and do not perform desired functions properly. This leads to secretion of excess amount of insulin leading to hyperinsulinemia. It is pretty common in PCOS and can happen because of obesity, lack of physical activity, and even genetics. As insulin is associated with so many metabolic processes in the body, increase in its levels can lead to complications which present themselves as various symptoms. It is linked to excess androgens in the body, obesity, cardiovascular diseases, atherosclerosis or buildup of fats in the artery walls that makes them hard and narrow. Studies also revealed dysregulation of steroidogenesis in ovaries, which is involved in producing the sex hormones. As ovaries start producing more androgens, the ovarian follicles get arrested and are not able to mature, leading to lack of ovulation. All these processes result in hirsutism, lack of periods, baldness and hair thinning, fat accumulation, and even type 2 diabetes.
There is a notion among the masses that PCOS is always associated with obesity. This can be agreed upon that mostly women who suffer from the disorder are obese, but there are many who aren’t part of that pack. These women belong to the lean type of PCOS. Lean PCOS consists of women with normal BMI or Body Mass Index. The symptoms between the two groups may not differ much. Both of these groups are found to have more insulin resistance as compared to their respective controls. In some studies, insulin levels were found to be normal in lean PCOS patients, but they did possess excess androgen production. They are found to have disturbed metabolism and more visceral fat as compared to their normal counterparts. Thus, obesity could be considered one of the possible symptoms of PCOS, however, since it is not present in all women with the syndrome, obese women can be considered to be more vulnerable to various complications of PCOS in comparison to the lean ones.
Is there any cure for it? Unfortunately, as many of you may know, there isn’t one. But yes, there are medications that can help keep the symptoms under control. Medicines like metformin make the body more sensitive to insulin levels. It also helps to reduce levels of androgens and cholesterol. Oral contraceptives help regularize menstrual cycle, and reduce the level of androgens, eventually, reducing hirsutism and acne. Most importantly, one needs to bring about certain lifestyle modifications. It includes exercises for physical and mental well-being, consumption of certain food items and avoiding others as much as possible. These can be different for the lean and obese types. Lifestyle changes are considered to be paramount in managing PCOS and we will be digging into it in the coming episodes!
References
Barrea, L., Frias-Toral, E., Verde, L., Ceriani, F., Cucalón, G., Garcia-Velasquez, E., Moretti, D., Savastano, S., Colao, A., & Muscogiuri, G. (2021). PCOS and nutritional approaches: Differences between lean and obese phenotype. Metabolism Open, 12, 100123. https://doi.org/10.1016/j.metop.2021.100123
Dawood, A., & Goyal, M. (2017). Debates regarding lean patients with polycystic ovary syndrome: A narrative review. Journal of Human Reproductive Sciences, 10(3), 154. https://doi.org/10.4103/jhrs.jhrs_77_17
Guzick, D. S. (2004). Polycystic Ovary Syndrome. Obstetrics & Gynecology, 103(1), 181–193. https://doi.org/10.1097/01.aog.0000104485.44999.c6
Insulin Resistance & Prediabetes. (2021, November 17). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance
Khan, K. A., Stas, S., & Kurukulasuriya, L. R. (2006). Polycystic Ovarian Syndrome. Journal of the CardioMetabolic Syndrome, 1(2), 125–132. https://doi.org/10.1111/j.1559-4564.2006.05675.x
NHS website. (2021, August 17). Polycystic ovary syndrome. Nhs.Uk. https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/
Polycystic ovary syndrome (PCOS) – Symptoms and causes. (2020, October 3). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439
Polycystic Ovary Syndrome Support Groups Are Helpful. (n.d.). PCOS Awareness Association. https://www.pcosaa.org/overview
Toosy, S., Sodi, R., & Pappachan, J. M. (2018). Lean polycystic ovary syndrome (PCOS): an evidence-based practical approach. Journal of Diabetes & Metabolic Disorders, 17(2), 277–285. https://doi.org/10.1007/s40200-018-0371-5
Wikipedia contributors. (2021, November 14). Insulin. Wikipedia. https://en.wikipedia.org/wiki/Insulin
Wolf, W., Wattick, R., Kinkade, O., & Olfert, M. (2018). Geographical Prevalence of Polycystic Ovary Syndrome as Determined by Region and Race/Ethnicity. International Journal of Environmental Research and Public Health, 15(11), 2589. https://doi.org/10.3390/ijerph15112589
. . .
Writer

Sreelakshmi S Kumar
Sreelakshmi is pursuing her undergraduate course degree in Zoology from Fergusson College, Pune. The field of Immunology and Virology interests her the most. She harbours her love for science and teaching inside her, and she wishes to teach in the future. Dancing, reading and calligraphy are some of her leisure activities and she is a big foodie too!
Illustrator

Aishwarya Girish
Aishwarya is an undergraduate pursuing her degree in B.E Biotechnology from Ramaiah Institute of Technology, Bangalore.